Using Data to Modernize the Medical Back Office
March 11, 2020
Kim Woofter, RN, and Robin Zon, MD, FACP, FASCO
Author BiosDisclosures
Ms. Kim Woofter
Article Highlights
Rising costs, declining reimbursements, and increasing operational complexity have resulted in more independent practices being absorbed into health systems.
The experiences of Michiana Hematology Oncology, PC in implementing data to streamline and enhance back-office processes by leveraging technology to improve efficiencies and redirect staff skills provides a case study for how to modernize the medical back office.
Cancer care options continue to evolve at a rapid pace due to innovation in diagnostics, therapeutics, and value-based care delivery models. However, the business side of health care has not kept pace. Oncology providers, perhaps more than other specialists, feel the pressure of rising costs, declining reimbursements, and increasing operational complexity. In fact, 58% of oncology practices specifically cite payer pressures as a top concern.1 Although the health care system needs to be cost-efficient while providing more value, the increasing complexity to run a practice is not sustainable in this current environment.
Our own experiences at Michiana Hematology Oncology (MHO), PC provides a potential framework on how to use data to modernize the medical back office and improve the work environment in a cost-efficient way. Herein, we describe our choice to implement a new initiative, explore some of the benefits as well as the challenges, and discuss, ultimately, how technology can not only improve but enhance your practice.
Dr. Robin Zon
Practice Background
MHO is the largest team of board-certified oncologists in Northern Indiana. The physician-owned practice has 21 providers, including 12 medical oncologists, four radiation oncologists, and five advanced practice nurses. The practice has eight locations and continues to expand with additional physicians and locations throughout north and northwest Indiana.
MHO provides integrated and comprehensive medical and radiation oncology services under one roof, including nutritional consults, chemotherapy, radiation therapy, and 24-hour oncology-certified nursing assistance. Our practice and physicians have earned a national reputation for leadership in patient advocacy, innovation in clinical operations, and ASCO leadership.
Why Implement Change: A Call to Action
Rising costs, declining reimbursements, and increasing operational complexity have resulted in more independent practices being absorbed into health systems. We strongly believe that MHO can provide the most cost-effective, high-quality, and comprehensive cancer care as an organization where every team member focuses exclusively on caring for and curing patients with cancer. However, the stark reality of our balance sheet showed that our practice was unsustainable if we did not find ways to streamline our operations and reduce the cost to support services that benefit patients beyond the care team’s direct touch.
With rising costs and reimbursement trends working against us, we could see that we needed to act urgently in order to preserve our practice. In 2016, we made a commitment to streamline and enhance our back-office processes by leveraging technology to improve efficiencies and redirect the skills of the staff.
Our journey of change started with staff and processes. After spending 18 months reorganizing our back-office teams, processes, and workflows, we saw real gains in productivity and financial outcomes. However, we realized that we had just explored the tip of the iceberg, and our team needed technology to work harder so they could work smarter. However, the technology to increase back-office productivity while lowering cost was not on the market. To answer this need, our practice chose to drive change and innovation by investing in developing our own technology to solve our problems.
Where to Begin: Evaluating Problems
One major problem we identified was not optimally collecting due reimbursements. This was, in part, due to the lack of a comprehensive picture of our fee schedules across all payers and to our lack of staff and time to audit our billing and payment transactions. Another challenge was understanding and managing our drug financials—ranging from purchasing to contracting with all parties (manufacturer, distributor, and payer) as well as pharmacoeconomic discussions within the practice.
Consequently, we started with fee schedule management as the foundation to understanding the financial performance of the practice. We dedicated people, time, and other resources to fully understand what our fee schedules were for every payer and every Current Procedural Terminology (CPT) code each quarter. This was time intensive, as most fee schedule capture has to be done manually and for each CPT code individually. By building this foundation, we were able to integrate technology and automation that now capture and analyze our fee schedules. This technology eliminates human error, allows us to scale our work across all payers/fee schedules, and reduces staff time involved in the process by nearly 90%.
Next Steps: Using Technology to Streamline Revenue Cycle
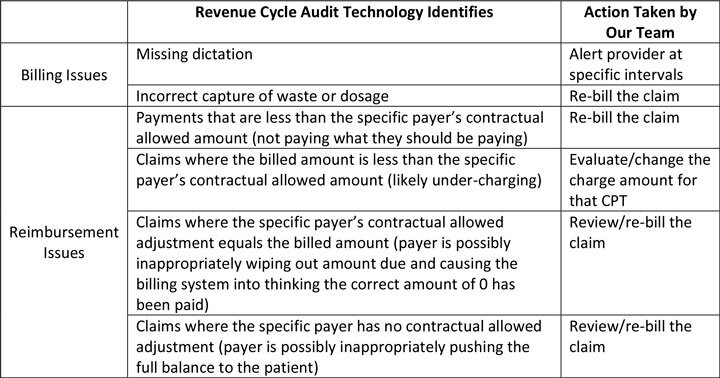
The next steps focused on identifying and then capturing missing reimbursement by creating a tool that audits 100% of our billed transactions. These audits range from simple analyses within one system (electronic medical record [EMR] or practice management/billing system) to more complex ones that look across multiple platforms (EMR, practice management system, and drug dispensing system). The technology then creates prompts for action to specific people within the practice for a variety of situations in which we may be missing a revenue opportunity (Table 1).
Table 1.Abbreviation: CPT, Current Procedural Terminology. View larger
We immediately began identifying billing issues resulting from missing dictation, incorrectly capturing billable waste, and process gaps within our revenue cycle team. There was an immediate revenue effect by identifying these issues, as we could re-bill any claims that occurred within the last 12 months, which now went to our bottom line (Table 1). In addition, the tool highlighted areas both within our billing team and within our clinical operations where we had opportunities to change processes and train staff, allowing us to largely eliminate these billing issues.
Once we had successfully improved our billing processes, we focused on identifying clean claims (claims that were billed correctly) but were reimbursed incorrectly. Now that we had a clearer picture of what we should be paid for every transaction, through our actively managed fee schedule data, we could identify the gaps in reimbursement between what we should be paid and what we were being paid. After deploying this technology, we were astonished to find how much revenue we were missing due to reimbursement errors.
The biggest gain for our practice was identifying payments that did not match the contractually allowed amount. In some cases, the payer shows a contractual allowed adjustment that equals the entire charge amount, which resulted in no payment and our billing system showing that there was no balance owed. In others, the payment was just less than it should be because of an incorrect fee schedule amount or incorrect dosage being applied by the payer. Importantly, we discovered with most of these reimbursement issues that once identified, we could re-bill and capture the missing reimbursement. In many cases, correcting these issues was the difference between underwater treatments (i.e., treatments for which reimbursements do not cover costs) and now being able to cover our costs and our overhead (Table 1).
The technology continues to identify reimbursement issues regularly, as payer reimbursement is still flawed. But now we have the tools in place to quickly identify and correct errors, and the financials of the practice have benefitted significantly.
From a clinical operations standpoint, we are now utilizing the technology to improve quality of care by comparing drug dosage across patients’ charts, our dispensing system, and our billing system. This has helped us identify issues, enabling us to make corrections and to improve processes and staff training. We have also identified cases in which dispensing practices were not consistent with our practice protocols, resulting in corrective action plans (Table 2).
Table 2.Abbreviation: NCCN, National Comprehensive Cancer Network. View larger
Blind Spots: Understanding and Actively Managing Drug Financials
One blind spot for our practice was quantifying financial management related to drug purchasing and use. We identified a need to streamline our purchasing processes and be more strategic about how and what we buy. By analyzing drug costs, purchasing patterns, and inventory management, we leveraged these data in negotiations with distributors and manufacturers. In addition, we became more efficient in managing inventory and ordering across our multisite practice. Notably, our physicians were highly engaged in better understanding drug financials and used clinical expertise primarily in choosing drug and treatment options. Empowering our provider clinical expertise with the financial data enabled a more productive pharmacoeconomic discussion within the practice. More broadly, the transparency around both quality and financial data helped us culturally focus on value-based care.
All parties—patients, providers, payers, and other stakeholders on the “business” side of health care—agree on the importance of balancing quality and cost in health care delivery. There is even considerable agreement on the way clinical decision support technology tools, including pathways , can help drive value-based decision-making.2 However, financial visibility is an often-missing piece for the clinician at time of decision-making. To encourage value-based decision-making, we built a mobile application allowing physicians to see payer-specific data in choosing least-costly alternatives when regimens are equally effective.
All providers in our practice agreed that we should know if a treatment plan is underwater. Our providers are committed to taking care of patients while providing the best care but will not be able to do so if reimbursements do not cover costs. To identify situations where we were underwater on treatments, we built another audit tool that looked at all scheduled treatments and the payer-specific financials associated with those treatments. The tool alerts our back-office team of these cases, and our back office informs the physician of the issue and any related details on treatment options (Table 2).
Importantly, financial data are not used to drive treatment planning. Rather, the technology developed generates data to drive more efficient back-office processes and more effective negotiations with our supply partners while arming our physicians with the financial data needed to inform value-based treatments. The information is a data point intended to complement evidence-based clinical knowledge. Ultimately, the physician makes a high-quality, evidence-driven decision around what is the best care for the patient.
Moving Forward
The health of our practice has improved significantly over the past 3 years. This is evident when looking at our back-office metrics (Table 3). We are capturing contractually due reimbursement previously underpaid and in a timely manner. We have seen significant improvement in the productivity and efficiency of our back office, which has translated to lower costs to run the practice. We are spending more cost effectively on drugs, and our drug utilization across the practice reflects a conscious and value-driven philosophy.
Table 3.Abbreviations: RCM, revenue cycle management; FTE, full-time employee. View larger
However, we acknowledge that our success to date is the beginning of an ongoing journey. Next steps include automating referral and intake analytics, and real-time Key Performance Indicator reporting for our physicians.
Ultimately, we envision a future thriving in value-based health care, where technology not only informs high-quality point of care clinical decision-making, but it also enables patients to receive the best-value care that they want and deserve.
Ultimately, we envision a future thriving in value-based health care, where technology not only informs high-quality point of care clinical decision-making, but it also enables patients to receive the best-value care that they want and deserve. Technology will enable our team to focus our time and energy on patient care and minimize time spent on the business of running a practice. Furthermore, this technology will preserve our practice as we continue to strive to provide the highest-quality and lowest-cost cancer care in the region.
References
State of Oncology Practice in America, 2018. American Society of Clinical Oncology. asco.org/sites/new-www.asco.org/files/content-files/blog-release/pdf/2018-SOCCA-Census-Article-Infographic-Web.pdf. Accessed January 28, 2020
Zon R, et al. Determining Value and Projecting the Future of Clinical Pathways: Part 2. Journal of Clinical Pathways. journalofclinicalpathways.com/news/determining-value-and-projecting-future-clinical-pathways-part-2. Published December 3, 2019. Accessed January 28, 2020.